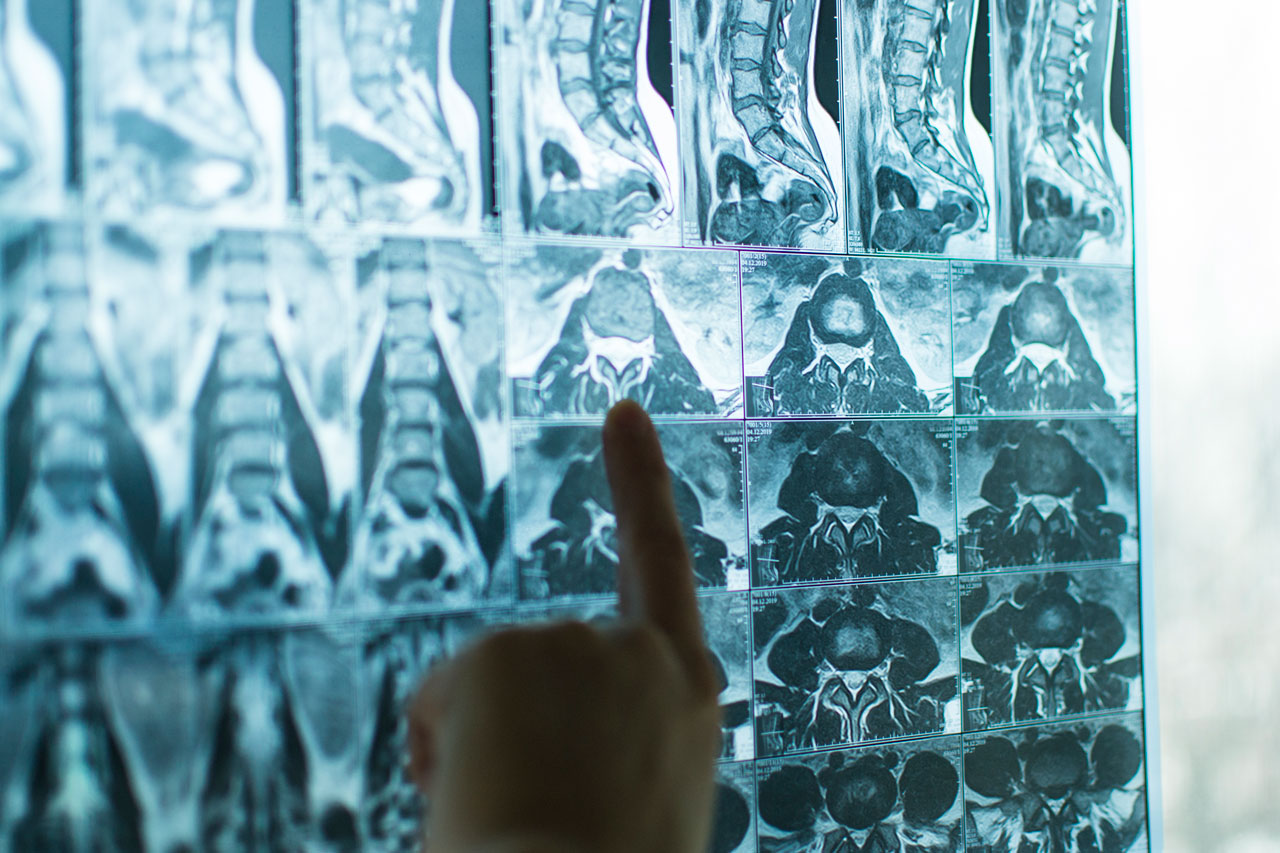
Many people living with Spinal Cord Injury (SCI) find that they have some degree of alteration or loss of their bowel function and control. This condition is usually referred to as neurogenic bowel dysfunction and occurs as a result of the disruption of communication between the brain, spinal cord and nerves that control the bowel.
Neurogenic bowel dysfunction may cause constipation in some people and bowel incontinence in others. In either situation, persons with neurogenic bowel dysfunction seek treatment and techniques to better control their bowel habits to either relieve constipation or to achieve continence. Better understanding of one’s bowel habits and achieving bowel continence is important to feel secure and confident to complete social activities without the worry of continence accidents.
Researchers at Neuroscience Research Australia (NeuRA) are investigating ways to improve bowel function in people with a spinal cord injury. Although over the years many treatments have attempted to improve bowel function in patients with SCI, most have not made a large difference.
One area that has shown promising results is the use of an implanted device called a sacral anterior root stimulator (SARS). This device was initially developed to improve bladder function. It was thought that the SARS could also help to improve bowel function because the colon, rectum, anal sphincter and bladder share some nerve roots.
The first SARS device was implanted in a person with SCI by Brindley et al. in 19761. Since then, more than 2,000 devices have been successfully implanted in patients around the world. Reviews of these devices have shown varied success for some people; with reports of shorter bowel management times and less need for manual interventions2. However, there can be side effects and complications from the surgery, as well as significant financial costs.
NeuRA researchers are now investigating the use of a non-invasive stimulation device that does not require surgery to improve bowel function. The details of this investigation are provided in the volunteer information sheet here. Should you be interested in participating in the investigation, please contact Mr. Keith McNaughton, Research Assistant, NeuRA, on 0416 598 885 or email at k.mcnaughton@neura.edu.au.
Research Links:
- Brindley, G. The first 500 patients with sacral anterior root stimulator implants: general description. Spinal Cord32, 795–805 (1994). https://doi.org/10.1038/sc.1994.126
- Vallès M, Rodríguez A, Borau A, Mearin F. Effect of sacral anterior root stimulator on bowel dysfunction in patients with spinal cord injury. Dis Colon Rectum. 2009;52(5):986-992. doi:10.1007/DCR.0b013e31819ed459